Halifax neonatologist to lead national research project on premature babies
Patent ductus arteriosus affects about half of extremely premature babies — and there's no national treatment practice
caption
Dr. Souvik Mitra is a neonatologist at the IWK Health Centre.A Halifax-based neonatologist is leading a national team of researchers looking into a condition that impacts babies born very prematurely.
In January, the Canadian Institute of Health Research (CIHR) awarded a national team led by IWK Health Centre neonatalogist Dr. Souvik Mitra a $313,652 grant to compare different medications used in the treatment of patent ductus arteriosus.
Patent ductus arteriosus (PDA) is a heart condition that occurs in premature babies when a blood vessel, ductus arteriosus, doesn’t close after birth.
It’s common in babies who are born at less than 33 weeks gestation, but the condition is worse in those born at less than 29 weeks.
The average gestation period in humans is 40 weeks, and a baby born at less than 37 weeks is considered premature.
Mitra is the research project’s team leader. He said about 25,000 to 30,000 babies are born prematurely in Canada each year.
“About half of extremely preterm infants who are born in Canada have this condition. And about two-thirds of them so, about 60 per cent of those who are diagnosed, need some form of treatment,” Mitra said in an interview.
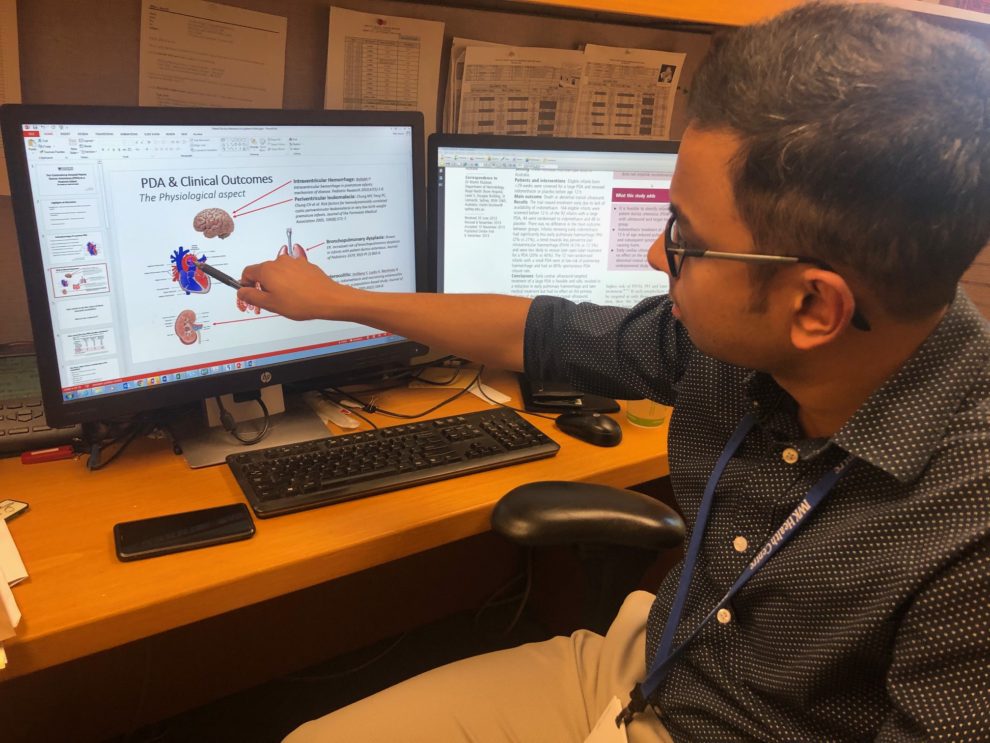
caption
Mitra pointing to PDA on a diagram of a heart.He said if this condition is not well-treated, it could lead to organ malfunction and ultimately the death of the baby.
Mitra said ibuprofen and Indomethacin, both anti-inflammatory drugs, are the two common medications used in treating PDA in Canadian medical centres, but there’s a variation in practice.
He said some of the medical centres use the standard dose of ibuprofen, some use a higher dose of ibuprofen, and others use Indomethacin.
“That’s a big problem because you want one unified treatment across the country,” he said.
Mitra said because there is so much treatment variation across the country, he wanted to compare the outcomes of the medications on preterm babies.
“Some believe that ibuprofen causes certain complications while others don’t,” he said, adding none of the three methods totally work.
“So, the balance is the degree of the benefit that I get versus the harms that I’m going to incur because of this medication,” he said.
One step forward, two steps back
One of Mitra’s IWK patients, Knox Hann, was born prematurely in 2016 at just 24 weeks.
Nick Hann, Knox’s father, said the doctors tried to close his son’s PDA many times through medications, but nothing worked.
He described it as an emotionally draining experience for him and his wife, Lisa. Hann and his wife were in the neonatal intensive care unit for 98 days.
“It was one step forward, two steps back because of that, so he had to have the PDA ligation, the surgery,” Hann said.
There were complications after the surgery.
“If there’s a possibility of avoiding the surgery and able to manage it in other ways, it’ll be very important and beneficial just for the fact that a baby that small doesn’t have to go in and undergo a surgery,” said Hann.
Knox is now three years old and attending daycare in Prince Edward Island, and Hann said he’s grateful to Mitra and his team for their help during that period.
“He’s just a normal little boy,” Hann said.
caption
Three-year-old Knox Hann.There are 31 major centres in Canada that treat extremely premature babies. Of those, 20 will be participating in Mitra’s research.
The research methodology will be what’s called a comparative effectiveness using real-world data. This method is new and useful in determining the extent to which the drugs work when they’re used in a real-life clinical setting.
“We know what the other factors are that could affect these outcomes and we’ll be collecting data on those outcomes as well and compare and account for that in the analysis,” he said.
Mitra said they intend to achieve a sample size of 1,100 babies over a period of three years.
“Whenever your numbers are limited, it is more difficult to find out very concrete answers to those problems,” he said.
‘We never want to get to surgery’
Mitra said PDA treatment can also lead to other health complications, like side effects from the medications.
“In trying to treat one problem, you’re introducing five different problems,” he said.
“We never want to get to surgery. So, you want to give them the medication that works, that has the highest chances of working right away, but with the least side effects.”
He said the bigger picture of the research is the impact the well-being of a baby who survived PDA has on the family as well as on society.
“Something that is extremely underappreciated is the impact of prematurity on the society,” said Mitra.
According to a January 2018 article in the Canadian Medical Association Journal (CMAJ), preterm birth — the leading cause of infant death, cerebral palsy and disability — costs the Canadian health care system approximately $8 billion per year.
Mitra said it’s not just about these babies surviving, it’s about them living without lifelong complications from a poorly-treated PDA condition.
“We just don’t talk about survival with parents, we talk about intact survival,” Mitra said.
He said his new goal in researching these medications is having babies survive PDA without major disabilities.
About the author
Seyitan Moritiwon
Seyitan is a journalism student at the University of King's College. She hung her lab coat after her degree in microbiology to start a career...

T
Tari
S
Sabrina
T
Thelma
i
ike
O
Omeyimi