HEALTH
Transgender community seeks better-informed doctors
Specialists look to family physicians to help with gender-affirming hormone therapy

caption
Syd Fraser had to wait nine months in order to see a specialist to start gender affirming hormone therapy
caption
Syd Fraser had to wait nine months before he could start gender-affirming hormone therapy.Transgender people in Nova Scotia are waiting up to a year to receive gender-affirming hormone therapy.
“It can be very difficult to find doctors who are knowledgeable with trans issues and comfortable with trans people,” says Syd Fraser a, 21-year-old transgender man living in Halifax.
Fraser started his hormone treatment in 2014. He was referred to an endocrinologist, a doctor specializing in diagnosing and treating hormone imbalances, but had to wait nine months for his appointment. In most cases, patients have to wait up to a year to be seen by a specialist.
“It was a lot of waiting and a lot of uncertainty about when I’d be seen (or) if I’d be seen, which can make you feel a little bit helpless,” says Fraser.
“I just have to wait around till someone deems me worthy, which is not great for your mental health.”
Gender-affirming hormone therapy is the primary medical treatment for transgender people, according to the World Professional Association for Transgender Health. The therapy allows individuals to take hormones, such as testosterone, to develop characteristics of the gender the individual identifies as.
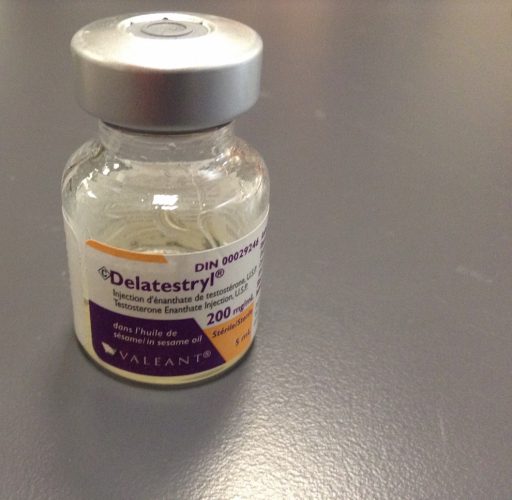
caption
This is a type of hormone used for gender-affirming hormone therapy.In Nova Scotia, family physicians or nurse practitioners working closely with family doctors and are able to prescribe gender-affirming hormones to patients. The therapy is initiated through informed consent, since the doctor already has a relationship with the patient.
Informed consent means “patients who are able to understand risks and benefits and the realistic expectations” of hormone therapy, says Kolten MacDonell, primary health care coordinator for prideHealth, which is part of the Capital Health division of the Nova Scotia Health Authority.
In most cases family physicians will refer patients looking for gender-affirming hormone therapy to a specialist or to the Halifax Sexual Health Centre, a clinic specializing in sexual and reproductive health care and education.
Once referred, individuals have to undergo a psychosocial gender transition readiness assessment designed by the World Professional Association for Transgender Health.
The assessment helps determine if the patient is ready, “in terms of having being able to consent and understand that this is the appropriate health service and that they are making an informed decision,” says MacDonell.
Wait times to get the readiness assessment through medial insurance provided by the government can be anywhere from 12 to 18 months. Private insurance does not pay for costs such as psychologists, who can help with this process.
This is one of the main reasons patients are facing such long wait times.
Emma Rose, clinic coordinator at the Halifax Sexual Health Centre, says more professionals should be trained to provide gender-affirming hormone therapy, such as family doctors.
“I think the hesitation is some doctors don’t have the knowledge or the skill to be able to provide the hormones,” she says.
Doctors Nova Scotia, the profession’s provincial association, would not comment on this issue.
PrideHealth works closely with family doctors across the province to train them in comprehensive care and offers an online Trans Health Guide.
Doctors need to gain more experience working with transgender patients, says Rose.
There needs to be an, “’I’m wanting to learn how to do this'” attitude, she says. “‘I want to help my patients and I’m just going to start learning and networking with doctors who have been doing it a little bit longer.’”
There are other barriers in Nova Scotia as well, especially for patients who live in rural areas. Many people looking for hormone therapy have to travel to Halifax, where most specialists are based.
“There is definitely work that needs to be done to make the service more accessible and prideHealth is working closely with family physicians to support them in providing gender-affirming therapy in the person’s medical home,” says MacDonell.

